Introduction
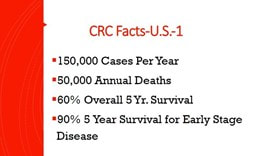
Colorectal Cancer (CRC) is a lethal and yet preventable disease both nationally and worldwide. There are roughly 150,000 cases diagnosed yearly with 50,000 annual fatalities in the United States. The overall 5 year survival for this diagnosis is 60 percent but when discovered at an early stage (Stage A or B ) survival rate jumps to 90 percent making strategies that enable early detection so vital. Physicians and Public Health officials are dismayed that upwards of 35 percent of the eligible population does not participate in any CRC screening programs. The reasons for this are complex and include lack of access to testing for vulnerable and low-income communities, embarrassment and fears about testing and lack of a systematic approach to screening by health care providers. Nonetheless, there has been a gradual decrease in CRC morality in the United States over the past two decades whereas other developed countries have seen a rise in CRC. This trend can at least partly be attributed to more robust screening protocols in the U.S. Unlike screening for Breast and Prostate Cancer, CRC screening can prevent the development of cancer in the first place by employing colonoscopic polypectomy to short circuit the progression of precancerous lesions to invasive CRC.
Epidemiology
There is significant global variation in the incidence of CRC with North America, Europe, Australia and New Zealand having high rates of disease and Africa along with South Asia having the lowest rates. Dr. Dennis Burkitt, a surgeon in the British Medical Service serving overseas during the post-World War II era, observed that colonic diseases such as diverticulitis and CRC were rare among Africans. He attributed this to lack of fiber intake in the western diet. Population studies suggest that offspring of immigrants who move from low incidence areas for CRC to high areas assume the rates of their adopted land suggesting major environmental influences in CRC development.
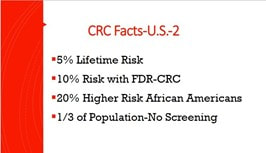
The lifetime risk for colon malignancy in the U.S is 5 percent. It should be noted that men have a 20 percent higher incidence of CRC and African Americans have a 20 percent higher incidence than Caucasians and are more likely to be diagnosed at a more advanced stage. First Degree Relatives (FDR)of patients with CRC have double the risk of CRC. It should be noted that 70 percent of CRC occurs in individuals with no family history (FH) of CRC or genetic syndromes. About 30 percent of patients with CRC have a FH of CRC or - less frequently - have a genetic predisposition such as Lynch Syndrome and Hereditary Polyposis Syndrome.
The majority of CRC arise from adenomas that undergo molecular changes that progress to malignant neoplasm– a process that may take upwards of 10 years. Approximately 30 percent of CRC have Sessile Serrated lesions which more often occur in the right colon, are sometimes flat and harder to detect on colonoscopy and likely have a more aggressive biology.
Colorectal Cancer (CRC) is a lethal and yet preventable disease both nationally and worldwide. There are roughly 150,000 cases diagnosed yearly with 50,000 annual fatalities in the United States. The overall 5 year survival for this diagnosis is 60 percent but when discovered at an early stage (Stage A or B ) survival rate jumps to 90 percent making strategies that enable early detection so vital. Physicians and Public Health officials are dismayed that upwards of 35 percent of the eligible population does not participate in any CRC screening programs. The reasons for this are complex and include lack of access to testing for vulnerable and low-income communities, embarrassment and fears about testing and lack of a systematic approach to screening by health care providers. Nonetheless, there has been a gradual decrease in CRC morality in the United States over the past two decades whereas other developed countries have seen a rise in CRC. This trend can at least partly be attributed to more robust screening protocols in the U.S. Unlike screening for Breast and Prostate Cancer, CRC screening can prevent the development of cancer in the first place by employing colonoscopic polypectomy to short circuit the progression of precancerous lesions to invasive CRC.
Epidemiology
There is significant global variation in the incidence of CRC with North America, Europe, Australia and New Zealand having high rates of disease and Africa along with South Asia having the lowest rates. Dr. Dennis Burkitt, a surgeon in the British Medical Service serving overseas during the post-World War II era, observed that colonic diseases such as diverticulitis and CRC were rare among Africans. He attributed this to lack of fiber intake in the western diet. Population studies suggest that offspring of immigrants who move from low incidence areas for CRC to high areas assume the rates of their adopted land suggesting major environmental influences in CRC development.
The lifetime risk for colon malignancy in the U.S is 5 percent. It should be noted that men have a 20 percent higher incidence of CRC and African Americans have a 20 percent higher incidence than Caucasians and are more likely to be diagnosed at a more advanced stage. First Degree Relatives (FDR)of patients with CRC have double the risk of CRC. It should be noted that 70 percent of CRC occurs in individuals with no family history (FH) of CRC or genetic syndromes. About 30 percent of patients with CRC have a FH of CRC or - less frequently - have a genetic predisposition such as Lynch Syndrome and Hereditary Polyposis Syndrome.
The majority of CRC arise from adenomas that undergo molecular changes that progress to malignant neoplasm– a process that may take upwards of 10 years. Approximately 30 percent of CRC have Sessile Serrated lesions which more often occur in the right colon, are sometimes flat and harder to detect on colonoscopy and likely have a more aggressive biology.
Risk and Protective Factors
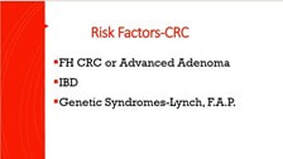
The most important risk factor for CRC is advancing age with over 90 percent of CRC cases diagnosed after age 40. The incidence of CRC rises steeply after age 60 and continues to rise with each successive decade. In addition to FH of CRC - patients with a FDR under age 60 diagnosed with advanced polyps have higher risk. Other risk factors include a personal history of CRC or colon polyps, Inflammatory Bowel Disease, and Pelvic Irradiation. Environmental factors that are linked to increased risk include smoking, moderate to heavy alcohol use, obesity, high intake of red meat, diets low in fiber, Diabetes, low levels of physical activity, low socioeconomic status and possibly post cholecystectomy state.
Reported protective factors include high physical activity, diets rich in fresh fruits and vegetables, supplemental calcium, Vitamin D, folate. Widespread use of low dose Aspirin for cardiac prophylaxis has been associated with a decrease in CRC in the middle-aged population - particularly men. NSAID prescription use has been shown to attenuate polyp development in high-risk patients with polyposis syndromes but are not advised routinely secondary to the occurrence of adverse effects such as gastrointestinal bleeding and kidney injury.
The most important risk factor for CRC is advancing age with over 90 percent of CRC cases diagnosed after age 40. The incidence of CRC rises steeply after age 60 and continues to rise with each successive decade. In addition to FH of CRC - patients with a FDR under age 60 diagnosed with advanced polyps have higher risk. Other risk factors include a personal history of CRC or colon polyps, Inflammatory Bowel Disease, and Pelvic Irradiation. Environmental factors that are linked to increased risk include smoking, moderate to heavy alcohol use, obesity, high intake of red meat, diets low in fiber, Diabetes, low levels of physical activity, low socioeconomic status and possibly post cholecystectomy state.
Reported protective factors include high physical activity, diets rich in fresh fruits and vegetables, supplemental calcium, Vitamin D, folate. Widespread use of low dose Aspirin for cardiac prophylaxis has been associated with a decrease in CRC in the middle-aged population - particularly men. NSAID prescription use has been shown to attenuate polyp development in high-risk patients with polyposis syndromes but are not advised routinely secondary to the occurrence of adverse effects such as gastrointestinal bleeding and kidney injury.
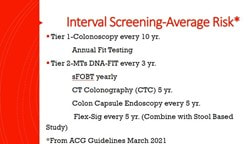
CRC Screening in Average Risk Patients
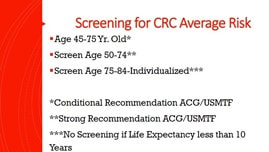
Average risks individuals refer to those who have no FH or personal history of CRC or polyps, no genetic syndromes, no history of IBD and no gastrointestinal symptoms. The prevailing consensus among major advisory bodies including the American Cancer Society, (ACS), United States Preventative Task Force (USPSTF) and the American College of Gastroenterology (ACG) advise that average risk patients begin screening at age 45 and continue to age 75. This has been motivated by a recent increase in the incidence in left sided colon cancer in younger patients in recent years. The USPSTF and ACG give “conditional” support recommendation citing weaker evidence of efficacy compared to beginning screening at age 50 where the evidence is more compelling. Decisions as to whether to continue screening after age 75 need to be individualized based on the patient’s comorbid conditions and previous screening history and not solely chronological age. As a rule of thumb, if a patient’s life expectancy is less than 10 years as harmful effects may outweigh benefits and should be discontinued.
Average risks individuals refer to those who have no FH or personal history of CRC or polyps, no genetic syndromes, no history of IBD and no gastrointestinal symptoms. The prevailing consensus among major advisory bodies including the American Cancer Society, (ACS), United States Preventative Task Force (USPSTF) and the American College of Gastroenterology (ACG) advise that average risk patients begin screening at age 45 and continue to age 75. This has been motivated by a recent increase in the incidence in left sided colon cancer in younger patients in recent years. The USPSTF and ACG give “conditional” support recommendation citing weaker evidence of efficacy compared to beginning screening at age 50 where the evidence is more compelling. Decisions as to whether to continue screening after age 75 need to be individualized based on the patient’s comorbid conditions and previous screening history and not solely chronological age. As a rule of thumb, if a patient’s life expectancy is less than 10 years as harmful effects may outweigh benefits and should be discontinued.
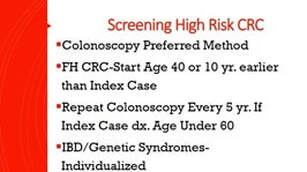
CRC Screening in High-Risk Patients
Colonoscopy is the recommended procedure for screening in high-risk patients. These include patients with a FDR with CRC or an advanced adenoma, IBD or a family history of a genetic syndrome. Screening should be carried out at age 40 or 10 years earlier than the diagnosis of the index case whichever is earliest. If the FDR was diagnosed under the age of 60- a 5-year interval follow up is advised. For those whose FDR were diagnosed at a more advanced age- a 10 year follow up is recommended provided the initial exam is negative. Screening intervals for IBD and Genetic syndrome patients are more frequent and individualized depending on the circumstances. Patients who have a personal history of colon polyps or CRC undergo “surveillance “colonoscopy and generally undergo colonoscopy every 3 to 5 years and are not considered in the “screening “category.
Colonoscopy is the recommended procedure for screening in high-risk patients. These include patients with a FDR with CRC or an advanced adenoma, IBD or a family history of a genetic syndrome. Screening should be carried out at age 40 or 10 years earlier than the diagnosis of the index case whichever is earliest. If the FDR was diagnosed under the age of 60- a 5-year interval follow up is advised. For those whose FDR were diagnosed at a more advanced age- a 10 year follow up is recommended provided the initial exam is negative. Screening intervals for IBD and Genetic syndrome patients are more frequent and individualized depending on the circumstances. Patients who have a personal history of colon polyps or CRC undergo “surveillance “colonoscopy and generally undergo colonoscopy every 3 to 5 years and are not considered in the “screening “category.
CRC Screening Methods
CRC screening modalities can be broadly divided into four basic columns: Endoscopy-which includes colonoscopy, flexible sigmoidoscopy, and capsule endoscopy, Imaging - CT Colonography, stool based studies which includes , Fecal Immunochemical Testing (FIT) Guaiac Based Fecal Occult Blood Test (gFOBT) and Multi- Targeted Stool DNA Tests with
Fit (MTsDNA /FIT- Cologuard) and serologic testing (Epi proColon 2.0) which detects septin 9 DNA hypermethylation. Though the serologic test is FDA approved, it is not recommended as a primary screening tool because of its lack of sensitivity and will not be further discussed. More narrowly screening can be further categorized as Step 1 - Colonoscopy and Step 2 which includes all other tests in that an abnormal result of all other tests must be followed up with colonoscopy. The ideal screening test should be sensitive and specific, inexpensive, easy to administer and safe. No one method checks all these boxes. The pros and cons of each of these methods will now be reviewed.
Stool-based Testing
F.I.T.
Fecal Immunochemical Test (FIT) testing requires one stool sample to be submitted annually and there are no dietary or medication restrictions. It detects human blood in the stool and is reported as positive for negative based on a quantitative reaction to reagent. The test has high sensitivity -80 percent and specificity -94 percent specificity in pooled studies.
Advantages - FIT is accurate, inexpensive, (20 dollars) and does not require bowel preparation or dietary restrictions. It is particularly helpful in low resource communities and receives high marks from all reviewing advisory societies.
Disadvantages- Results are optimal if the stool sample is processed within 24 hours as accuracy degrades over time and with high ambient temperatures. Best results are obtained if the test is done on an annual basis. Sensitivity for detecting precancerous adenomas is low.
Multitarget Stool DNA Tests with FIT (MTsDNA/FIT - Cologuard)
MTs DNA- FIT is composed of a molecular assay that detects KRAS and two other gene mutations associated with CRC. Gene amplification techniques are employed to test for markers for methylation for biomarkers for CRC- This is combined with traditional FIT testing and a full stool sample is collected. The exam is done every 3 years. Sensitivity for detecting CRC is high 92 percent but sensitivity is lower than FIT alone. Results are reported as positive or negative, so it is unclear which component of the test, MTsDNA or FIT, is responsible for the positive test.
Advantages – The exam is done at home with no bowel preparation, is non-invasive and annual
exams are not required. Sensitivity for CRC detection is high.
Disadvantages – The test is costly (several hundred dollars) and has lower specificity than FIT.
Overall MTsDNA/FIT is less cost effective than annual FIT testing. This study is not well suited for low resource communities. There is uncertainty with respect to how to follow up on a positive result in the setting of a negative colonoscopy. Sensitivity for detecting precancerous adenomas is superior to FIT but still relatively low compared to colonoscopy.
Guaiac-Based Fecal Occult Blood Test (g FOBT)
This method identifies hemoglobin in stool via a peroxidase reaction of impregnated paper slide- turning it blue on contact. This is the oldest of screening tests and requires 3 stool samples on successive days. Sensitivity is wide ranging (31- 79 percent) with one time use with a specificity of over 85 percent. Best practice is to do the exam on an annual basis. Multiple randomized controlled trials, when properly performed, reduces mortality from CRC. Various brands exist but it advised that high sensitivity Hemoccult Sensa be used.
Advantages – Examination is low cost (less than 20 dollars), reasonable sensitivity when properly performed and helpful in settings where resources are limited.
Disadvantages – The study is done on an annual basis and three separate stool studies are
provided which may make compliance difficult. Patients are advised to restrict intake of red meat during testing and avoid the use of NSAIDs and ASA. Accuracy degrades over time and cards are sent to the lab via mail frequently. For these reasons, FIT has largely replaced g-FOBT as the preferred low-cost stool-based screening test.
Visualization Screening Tests
Colonoscopy
Colonoscopy is often considered the “gold standard “when it comes to colorectal cancer screening. Sensitivity for detecting CRC or precancerous lesions over 10 cm is over 95 %.and 95 % specific. Pooled observational studies indicate a 68 percent reduction in CRC mortality for those screened. Examinations are performed every 10 years in average risk patients.
Advantages – The major advantage for colonoscopy has high sensitivity and specificity compared to other screening methods and provides diagnostic and therapeutic capabilities. Adenomas and Sessile serrated lesions can be removed endoscopically at the time of procedure thus disrupting the polyp to CRC progression.
Colonoscopy can detect flat, sessile lesions that frequently escape other screening tests. Moreover, a negative exam by a high performing endoscopist is associated with a low risk for CRC for the next 5-10 years. Despite high “upfront “ compares favorable for “years of life saved“ compared to other screening procedures i.e. mammography.
Disadvantages –Disadvantages include cost- (cost highest among all of screening methods- varies regionally - 800 dollars to several thousand dollars), extensive bowel preparation with possible dehydration and electrolyte imbalance, time off from work and need for anesthesia with attendant risks. Serious procedure related complications include colon perforation – (1 in1000- 2000), major bleeding post polypectomy and cardiopulmonary events related to anesthesia. Protective benefit of colonoscopy is highly operator dependent with outcomes dependent on quality measures such as the endoscopist’s adenoma detection rate and cecal withdrawal time. Adequacy of colonic preparation can be problematic particularly in the detection of flat right colonic lesions. Patients over 65 are at higher risk for procedure related complications. Canadian studies suggested that colonoscopy was not highly effective in preventing proximal or right sided CRC. It should be noted that examinations were frequently performed by primary care providers and general surgeons. And not gastroenterologist. Colonoscopy is not readily available in many low resource communities.
Flexible Sigmoidoscopy
The procedure is performed in the office setting frequently without sedation. The distal 40 -60 cm of the colon is examined. A five-year interval is recommended. The exam requires a limited bowel preparation. Mortality from CRC in studies is reduced by 50 % This result is primarily in the occurrence of left sided or distal colonic lesions.
Advantages - Their examination does not require sedation and time off from work. The bowel
preparation is limited Flexible Sigmoidoscopy is best done in conjunction in stool-based studies.
Disadvantages - Requires limited bowel prep. Sedation is not routinely administered and can be uncomfortable. It does not evaluate proximal colon lesions which are responsible for 50 % of advanced lesions particularly in older patients and females. Because of patient discomfort and guidelines advocating full colonoscopy, popularity of this test has declined.
CT Colonography
The examination is performed every 5 years for screening. Colorectal neoplasm detection of CRC and lesions over 1 cm in upwards of 90 percent in expert and high-volume centers. The procedure is low risk for complications and does not require sedation. It does require an extensive bowel prep much like that necessary for colonoscopy
Advantages - Non-invasive study, moderate costs, and good sensitivity. CTC is especially helpful for patients who are unable to have a full colonoscopy secondary to altered anatomy or are unwilling to undergo colonoscopy.
Disadvantages - A rigorous bowel preparation is required, radiation exposure and lower
sensitivity in detecting flat – right sided colon lesions. Positive results require follow up colonoscopy which makes this study a less cost-effective screening measure. The presence of extra colonic findings on imaging may lead to further unnecessary investigations. Published data on CTC were generated by high volume centers.
Community hospitals that do less frequent exams may have less optimal results.
Capsule Colonoscopy
Capsule Colonoscopy is a method of CRC screening approved for use by the FDA and European Medicine Agency as a screening tool. The sensitivity for detection polyps over 6 mm and CRC was 69 % with a specificity of 86 percent. The examination will detect the majority of CRC particularly with updated technology.
Advantages- - non- invasive –moderate cost - good sensitivity and specificity - helpful for
patients who are unable to have complete colonoscopy secondary to anatomic issues or unwilling to undergo colonoscopy.
Disadvantages – Full bowel preparation is required- Moderate cost. Abnormal results trigger full colonoscopy. This test is used more frequently in Europe and not widely available in the US.
Conclusions
CRC remains a major international and national health care challenge. Screening procedures are designed to detect early CRC and in the case of colonoscopy, prevent its development. Multiple options are available for screening, and it is often postulated that the best screening test is the “one that gets done.” The method chosen for CRC screening in the population is most often driven by patient preference, advice given by primary care providers, and cost considerations. The ACG advises that the most efficient and effective strategy for colon cancer screening is either annual FIT testing or Colonoscopy every ten years. Since FIT testing best
results are obtained when done on an annual basis, it requires diligence on behalf of both providers and patients. Proponents of MTs-DNA/FIT may disagree with this assessment.
Colonoscopy is the most sensitive and specific study in detecting CRC and premalignant polyps and providing therapeutic capability when these lesions are detected. Best outcomes occur when the procedure is performed by an examiner who scores high on quality metrics.
The bottom line is that CRC is largely a preventable disease. Advisory Boards recommend screening the general population between ages 45-75 based on evidence from multiple studies. Barriers to screening continue to exist and a primary determinant of who and how patients are screened is insurance status. Patients with private health insurance have higher screening rates compared to those with government sponsored insurance. It is not surprising that those with no health insurance have the lowest screening rates. Many African Americans and individuals with low socio-economic status have higher CRC mortality because of disparities in health system access to screening, diagnosis, and treatment. Most screening in the U.S. occurs on an “opportunistic basis” which is arranged at the discretion of a primary care provider or a request by patients to be screened. Organized screening processes are much more effective boosting CRC screening rates and include mail notification, email reminders, phone calls and utilization of EMR reminders. A study of Kaiser Permanente’s Northern California with 4 million members demonstrated a rise in screening rates from 38 percent in 2000 to 82 percent in 2015 by utilizing these measures. The effects of the COVID 19 Pandemic on screening in general and CRC are yet to be elucidated but no doubt will be deleterious and will challenge providers and patients going forward. March is colon cancer awareness month. Let us do our part in CRC screening advocacy as providers not only every March but throughout the calendar year.
CRC screening modalities can be broadly divided into four basic columns: Endoscopy-which includes colonoscopy, flexible sigmoidoscopy, and capsule endoscopy, Imaging - CT Colonography, stool based studies which includes , Fecal Immunochemical Testing (FIT) Guaiac Based Fecal Occult Blood Test (gFOBT) and Multi- Targeted Stool DNA Tests with
Fit (MTsDNA /FIT- Cologuard) and serologic testing (Epi proColon 2.0) which detects septin 9 DNA hypermethylation. Though the serologic test is FDA approved, it is not recommended as a primary screening tool because of its lack of sensitivity and will not be further discussed. More narrowly screening can be further categorized as Step 1 - Colonoscopy and Step 2 which includes all other tests in that an abnormal result of all other tests must be followed up with colonoscopy. The ideal screening test should be sensitive and specific, inexpensive, easy to administer and safe. No one method checks all these boxes. The pros and cons of each of these methods will now be reviewed.
Stool-based Testing
F.I.T.
Fecal Immunochemical Test (FIT) testing requires one stool sample to be submitted annually and there are no dietary or medication restrictions. It detects human blood in the stool and is reported as positive for negative based on a quantitative reaction to reagent. The test has high sensitivity -80 percent and specificity -94 percent specificity in pooled studies.
Advantages - FIT is accurate, inexpensive, (20 dollars) and does not require bowel preparation or dietary restrictions. It is particularly helpful in low resource communities and receives high marks from all reviewing advisory societies.
Disadvantages- Results are optimal if the stool sample is processed within 24 hours as accuracy degrades over time and with high ambient temperatures. Best results are obtained if the test is done on an annual basis. Sensitivity for detecting precancerous adenomas is low.
Multitarget Stool DNA Tests with FIT (MTsDNA/FIT - Cologuard)
MTs DNA- FIT is composed of a molecular assay that detects KRAS and two other gene mutations associated with CRC. Gene amplification techniques are employed to test for markers for methylation for biomarkers for CRC- This is combined with traditional FIT testing and a full stool sample is collected. The exam is done every 3 years. Sensitivity for detecting CRC is high 92 percent but sensitivity is lower than FIT alone. Results are reported as positive or negative, so it is unclear which component of the test, MTsDNA or FIT, is responsible for the positive test.
Advantages – The exam is done at home with no bowel preparation, is non-invasive and annual
exams are not required. Sensitivity for CRC detection is high.
Disadvantages – The test is costly (several hundred dollars) and has lower specificity than FIT.
Overall MTsDNA/FIT is less cost effective than annual FIT testing. This study is not well suited for low resource communities. There is uncertainty with respect to how to follow up on a positive result in the setting of a negative colonoscopy. Sensitivity for detecting precancerous adenomas is superior to FIT but still relatively low compared to colonoscopy.
Guaiac-Based Fecal Occult Blood Test (g FOBT)
This method identifies hemoglobin in stool via a peroxidase reaction of impregnated paper slide- turning it blue on contact. This is the oldest of screening tests and requires 3 stool samples on successive days. Sensitivity is wide ranging (31- 79 percent) with one time use with a specificity of over 85 percent. Best practice is to do the exam on an annual basis. Multiple randomized controlled trials, when properly performed, reduces mortality from CRC. Various brands exist but it advised that high sensitivity Hemoccult Sensa be used.
Advantages – Examination is low cost (less than 20 dollars), reasonable sensitivity when properly performed and helpful in settings where resources are limited.
Disadvantages – The study is done on an annual basis and three separate stool studies are
provided which may make compliance difficult. Patients are advised to restrict intake of red meat during testing and avoid the use of NSAIDs and ASA. Accuracy degrades over time and cards are sent to the lab via mail frequently. For these reasons, FIT has largely replaced g-FOBT as the preferred low-cost stool-based screening test.
Visualization Screening Tests
Colonoscopy
Colonoscopy is often considered the “gold standard “when it comes to colorectal cancer screening. Sensitivity for detecting CRC or precancerous lesions over 10 cm is over 95 %.and 95 % specific. Pooled observational studies indicate a 68 percent reduction in CRC mortality for those screened. Examinations are performed every 10 years in average risk patients.
Advantages – The major advantage for colonoscopy has high sensitivity and specificity compared to other screening methods and provides diagnostic and therapeutic capabilities. Adenomas and Sessile serrated lesions can be removed endoscopically at the time of procedure thus disrupting the polyp to CRC progression.
Colonoscopy can detect flat, sessile lesions that frequently escape other screening tests. Moreover, a negative exam by a high performing endoscopist is associated with a low risk for CRC for the next 5-10 years. Despite high “upfront “ compares favorable for “years of life saved“ compared to other screening procedures i.e. mammography.
Disadvantages –Disadvantages include cost- (cost highest among all of screening methods- varies regionally - 800 dollars to several thousand dollars), extensive bowel preparation with possible dehydration and electrolyte imbalance, time off from work and need for anesthesia with attendant risks. Serious procedure related complications include colon perforation – (1 in1000- 2000), major bleeding post polypectomy and cardiopulmonary events related to anesthesia. Protective benefit of colonoscopy is highly operator dependent with outcomes dependent on quality measures such as the endoscopist’s adenoma detection rate and cecal withdrawal time. Adequacy of colonic preparation can be problematic particularly in the detection of flat right colonic lesions. Patients over 65 are at higher risk for procedure related complications. Canadian studies suggested that colonoscopy was not highly effective in preventing proximal or right sided CRC. It should be noted that examinations were frequently performed by primary care providers and general surgeons. And not gastroenterologist. Colonoscopy is not readily available in many low resource communities.
Flexible Sigmoidoscopy
The procedure is performed in the office setting frequently without sedation. The distal 40 -60 cm of the colon is examined. A five-year interval is recommended. The exam requires a limited bowel preparation. Mortality from CRC in studies is reduced by 50 % This result is primarily in the occurrence of left sided or distal colonic lesions.
Advantages - Their examination does not require sedation and time off from work. The bowel
preparation is limited Flexible Sigmoidoscopy is best done in conjunction in stool-based studies.
Disadvantages - Requires limited bowel prep. Sedation is not routinely administered and can be uncomfortable. It does not evaluate proximal colon lesions which are responsible for 50 % of advanced lesions particularly in older patients and females. Because of patient discomfort and guidelines advocating full colonoscopy, popularity of this test has declined.
CT Colonography
The examination is performed every 5 years for screening. Colorectal neoplasm detection of CRC and lesions over 1 cm in upwards of 90 percent in expert and high-volume centers. The procedure is low risk for complications and does not require sedation. It does require an extensive bowel prep much like that necessary for colonoscopy
Advantages - Non-invasive study, moderate costs, and good sensitivity. CTC is especially helpful for patients who are unable to have a full colonoscopy secondary to altered anatomy or are unwilling to undergo colonoscopy.
Disadvantages - A rigorous bowel preparation is required, radiation exposure and lower
sensitivity in detecting flat – right sided colon lesions. Positive results require follow up colonoscopy which makes this study a less cost-effective screening measure. The presence of extra colonic findings on imaging may lead to further unnecessary investigations. Published data on CTC were generated by high volume centers.
Community hospitals that do less frequent exams may have less optimal results.
Capsule Colonoscopy
Capsule Colonoscopy is a method of CRC screening approved for use by the FDA and European Medicine Agency as a screening tool. The sensitivity for detection polyps over 6 mm and CRC was 69 % with a specificity of 86 percent. The examination will detect the majority of CRC particularly with updated technology.
Advantages- - non- invasive –moderate cost - good sensitivity and specificity - helpful for
patients who are unable to have complete colonoscopy secondary to anatomic issues or unwilling to undergo colonoscopy.
Disadvantages – Full bowel preparation is required- Moderate cost. Abnormal results trigger full colonoscopy. This test is used more frequently in Europe and not widely available in the US.
Conclusions
CRC remains a major international and national health care challenge. Screening procedures are designed to detect early CRC and in the case of colonoscopy, prevent its development. Multiple options are available for screening, and it is often postulated that the best screening test is the “one that gets done.” The method chosen for CRC screening in the population is most often driven by patient preference, advice given by primary care providers, and cost considerations. The ACG advises that the most efficient and effective strategy for colon cancer screening is either annual FIT testing or Colonoscopy every ten years. Since FIT testing best
results are obtained when done on an annual basis, it requires diligence on behalf of both providers and patients. Proponents of MTs-DNA/FIT may disagree with this assessment.
Colonoscopy is the most sensitive and specific study in detecting CRC and premalignant polyps and providing therapeutic capability when these lesions are detected. Best outcomes occur when the procedure is performed by an examiner who scores high on quality metrics.
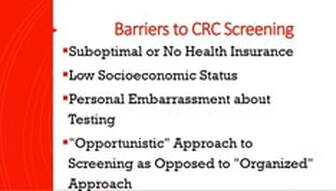
The bottom line is that CRC is largely a preventable disease. Advisory Boards recommend screening the general population between ages 45-75 based on evidence from multiple studies. Barriers to screening continue to exist and a primary determinant of who and how patients are screened is insurance status. Patients with private health insurance have higher screening rates compared to those with government sponsored insurance. It is not surprising that those with no health insurance have the lowest screening rates. Many African Americans and individuals with low socio-economic status have higher CRC mortality because of disparities in health system access to screening, diagnosis, and treatment. Most screening in the U.S. occurs on an “opportunistic basis” which is arranged at the discretion of a primary care provider or a request by patients to be screened. Organized screening processes are much more effective boosting CRC screening rates and include mail notification, email reminders, phone calls and utilization of EMR reminders. A study of Kaiser Permanente’s Northern California with 4 million members demonstrated a rise in screening rates from 38 percent in 2000 to 82 percent in 2015 by utilizing these measures. The effects of the COVID 19 Pandemic on screening in general and CRC are yet to be elucidated but no doubt will be deleterious and will challenge providers and patients going forward. March is colon cancer awareness month. Let us do our part in CRC screening advocacy as providers not only every March but throughout the calendar year.
Written by Jerome Burke. MD, FACG